Achilles tendon rupture: the best exercises to prevent it

- 1 What is the Achilles tendon?
- 2 Tendon rupture
- 3 What is the Achilles tendon?
- 4 When to be careful?
- 5 How to notice the breakup?
- 6 How to intervene?
- 7 How to prevent?
- 8
- 9
- 10
Achilles tendon: anatomical information
The name Achilles tendon dates back to Greek mythology.
The heel was the only part of the body where the hero Achilles was vulnerable: an arrow hit him exactly there, causing his death.
The Achilles tendon (Tendon calcaneus) connects the heel bone with the calf muscle (Musculus triceps surae). With a length of 20 to 25 centimeters and an average width of about 5 centimeters, it is the strongest tendon in the human body. It allows us to stand on tiptoe and push while running and jumping. It can be easily felt by palpating it through the skin just above the heel.
During sports (especially ball sports, running, jumping, football, and cycling), a force multiple of the body weight acts on the Achilles tendon.
Overview: What is a torn Achilles tendon?
A torn Achilles tendon is one of the typical sports injuries. The tendon, which connects the heel bone and the calf muscles, is particularly affected by sudden accelerations and sudden stops, which can generate so much stress that it causes massive injury or total rupture.
During a tendon rupture, the subject perceives a clear pop, like the sound of a whip, and immediate and intense pain. In addition, people affected by this type of injury report that it feels like someone has stepped on their tendon, causing a sharp stabbing pain in the lower calf. This pain is usually not as persistent as other injuries or accidents.
Subsequently, hematomas and probably hollows form over the heel, and functional impotence occurs, whereby it is no longer possible to push the foot or walk, at least on the toes.
A completely injured tendon almost always requires surgical procedures.
Achilles tendon rupture: epidemiology
A ruptured Achilles tendon is quite common: more than ten out of every 100,000 people contract it yearly, men up to ten times more often than women.
The age group between 30 and 60 is particularly affected since, with advancing age, signs of tendon wear are also present.
A rupture of the Achilles tendon is mainly caused by ball sports and most often affects untrained people and typically occurs in amateur athletes in the age group mentioned above.
Achilles tendon rupture: causes and risk factors
Injuries to the Achilles tendon are most common during sports, particularly ball sports, running, and other sports that involve jumping. It usually occurs due to an abrupt tightening of the tendon, for example, with activities that require rapid stop-and-go movements, sprinting, or jumping.
If the Achilles tendon tears, it is usually already damaged, e.g., due to aging. If the tendon is not sufficiently warmed and stretched before exercise, the risk of rupture is particularly high.
The Achilles tendon tissue’s wear and tear can start at a young age. In addition, people who are not physically active have a higher risk of tearing the Achilles tendon under stress since a low level of fitness means that the entire muscle-tendon system is less elastic and more prone to injury.
Risk factors for a ruptured Achilles tendon include:
- Advanced age;
- Muscle dysfunction;
- Male gender;
- Taking antibiotics (quinolones), anabolic steroids, and cortisone;
- Micro-injuries due to excessive exertion, e.g. during sport;
- Diseases such as diabetes mellitus.
Very rarely, direct violence, such as a knife cut or a kick with a cleated shoe, causes the Achilles tendon to rupture.
Achilles tendon rupture: symptoms
The main symptoms after an Achilles tendon rupture are:
- pain (which tends to disappear in the absence of stress),
- oedema and haematoma,
- limited movement.
Symptoms manifest themselves as time passes:
- immediately presented as a sharp stabbing pain in the lower calf that feels like being kicked in the tendon;
- the ability to walk and stand is immediately significantly reduced, so at the very least, it is not possible to lift oneself up on the toes of the affected foot, but even walking or leaning on the foot is difficult, if not impossible;
- there are palpable hollows and hematomas above the heel;
- edema in the calf and the back of the ankle.
In the case of these typical symptoms, the diagnosis is quite simple since a rupture of the Achilles tendon is already suspected.
Achilles tendon rupture: diagnosis
The diagnosis is usually simple and can be made unequivocally based on the typical event and symptoms. It is generally recognized quickly when the course of the injury is described. In addition, a depression can be palpated by touch, often visible under the skin above the Achilles tendon. As mentioned earlier, the clinical symptomatology of not being able to stand on tiptoe is crucial for diagnosing tendon rupture.
The so-called Thompson test provides further confirmation of an injured Achilles tendon: to do this, with the subject lying on his stomach, the affected leg is allowed to hang loosely. With the Achilles tendon intact, the toes move towards the sole of the foot by squeezing the calf muscles. If the tendon is torn, this reflex does not occur.
Imaging methods can contribute to the diagnosis:
-
- X-ray examination can exclude that parts of the bone are injured (bone avulsion).
- Ultrasound (ultrasound) of the Achilles tendon region helps to identify the location and extent of the injury and to check how far apart the ends of the ruptured tendon are.
- Magnetic resonance imaging (MRI) can be used to assess the tear more precisely. However, an MRI examination is not necessary for every affected person, but only if the tendon is partially injured.
Achilles tendon ruptures are usually treated on an outpatient basis with a conservative procedure in the case of partial ruptures or surgery in the case of complete or massive tears.
In the case of partial ruptures, conservative treatment with relief and immobilization of the foot is possible. For this, it is necessary to wear splints or special shoes.
In the case of a complete rupture, when the two ends of the tendon no longer touch, the tendon must be surgically sewn up.
Achilles tendon rupture: conservative treatment
If the ends of the lesion touch when the foot is lowered into the so-called equine position, the tendon may (rarely) be able to repair itself without surgery.
An ultrasound examination is used to determine whether the equine position is possible.
During the treatment period, the foot is stabilized with an orthosis or special insole, making initial resilience possible. Full resilience is slowly built up with early functional therapy and physiotherapy. Treatment is usually completed after six to eight weeks.
Achilles tendon rupture: surgical treatment
If the ends of the tear no longer touch when the foot is lowered, an operation is required. During the procedure, the two ends of the tear are sewn together.
The procedure is performed with a long incision of up to eight centimeters above the Achilles tendon or minimally invasive with small incisions. The procedure is performed under general anesthesia if the Achilles tendon is severely damaged and a tendon transplant is required.
The tendon tube is opened during the procedure, and the ends are sutured.
After the operation, the foot is immobilized. As soon as the wound has healed, early functional treatment and physiotherapy begin.
Scientific studies show that the healing rate with an operation is several percentage points higher than when the injury is only treated conservatively.
With surgery, there is a risk of wound infection; this can be reduced with new minimally invasive surgical techniques. Surgical therapy is preferred, especially in young, active patients.
Regardless of whether treatment is conservative or surgical, functional follow-up treatment, i.e., early constructive motor therapy, should follow.
In special shoes with raised heels and a rigid tongue, the leg can be loaded again with full weight-bearing after a short time. Physiotherapeutic treatment can begin within three weeks at the latest. Shoes or splints are usually no longer necessary six to eight weeks after the accident.
However, the calf muscles must be strengthened again with targeted training. Three to six months after the end of the treatment, the injured person can play sports again.
Course and prognosis
The course and prognosis of an Achilles tendon rupture are highly dependent on therapy.
If it is done professionally and there is consistent follow-up treatment, it is almost always possible to restore Achilles tendon capacity and ankle function.
This allows for regaining performance levels prior to the tendon injury.
However, this favorable prognosis does not apply to top athletes in the jumping and running disciplines: a torn Achilles tendon often means the end of their career, as they often fail to regain total physical and mental capacity despite subsequent therapy and treatment.
The risk of thrombosis of the leg veins increases after a ruptured Achilles tendon.
Achilles tendon rupture: how to prevent it?
Warming up, stretching before and after exercise, and avoiding sudden movements help prevent tendon injuries.
1. Train regularly. Rely on dedicated strength and endurance training, gradually increasing the load.
2. For untrained people or amateurs, avoid extremely fast, abrupt, and therefore heavy loads (e.g., in squash, tennis, and football), as these often lead to Achilles tendon ruptures.
3. Warm up the muscles, tendons, and joints before physical exertion.
4. Since an Achilles tendon rupture is an accident and, therefore, a sudden event, early diagnosis is not possible.
Exercises to prevent Achilles tendon injury
What is important about Achilles tendon exercises?
An Achilles tendon will only heal when it is ‘strained,’ i.e., when it is loaded.
So: exercises, exercises, exercises!
It all depends on the load level of the exercise: if the load is too low, the Achilles tendon reacts little or not at all. Therefore: high loads are required (90% of maximum voluntary contractility).
Duration and speed are also crucial, so it is better to exercise longer, i.e., stay longer in the stress phase and do fewer repetitions than shorter exercises with many repetitions (exercise duration of at least 6 seconds). The total duration of the loading phase is important, with the eccentric phase (stretching downwards) having to be considerably longer.
The chosen loading form (eccentric, concentric, isometric, slow resistance) is of secondary importance. Some scientists even say that it does not matter.
Achilles tendon exercises can cause pain, which should not be too high or even increase during or after the workout. So: exercise in pain, but without overdoing it.
To get an idea of how severe the pain is and to be able to classify the pain in a meaningful way, imagine a scale from 1 to 10 where:
1 = no pain,
10 = maximum pain.
Achilles tendon exercises should be between 3 and 5 on the pain scale. During the break, the pain sensation should be below 3.
Example of an ‘eccentric Achilles tendon training plan
- 3 sets of 15 repetitions
- Slow execution
- Rest 2 minutes between sets.
All exercises, once with a straight knee and once with a bent knee, 5 minutes rest between these two variations.
The load can be increased slowly by carrying a variable-weight backpack on your back and increasing it every week, always following the sensation of pain as a guideline: no more than 5 on the imaginary scale.
Caution: the higher the load, the more important it is to take a 36-hour break before the next training session. Before then, the Achilles tendon was still in the regeneration phase, and any new exertion would negate all efforts.
Heavy, slow endurance training has longer breaks between loads (3 times a week), which corresponds more to the idea that the Achilles tendon needs sufficient time to regenerate.
1. Eccentric stretching of the Achilles tendon
Exercise from the ground; the affected foot is not overstretched when lowered.
Step 1: on the floor with both feet;
Step 2: on the floor, on one foot on tiptoe;
Step 3: on the floor, lowering the affected foot.
2. Achilles tendon eccentric stretching exercise
Step 1: position the forefoot on the edge of a step with the affected leg.
Step 2: then stand up on tiptoe.
Step 3: Slowly lower the foot under the top edge of the step.
Variations on this Achilles tendon exercise: once with a straight knee and once with a bent knee.
3. Jumping on one leg
Simply jump across forward, sideways, or backward on the sole of your foot, then switch feet. Repeat 10 jumps 10 times with a 30-second break between sets.
4. Achilles tendon ‘slow heavy resistance training exercise’
Heavy, slow resistance training (should be done with or guided by a physiotherapist and then performed in a weight room/gym).
3 different exercises for the Achilles tendon, each with both legs.
3-4 sets with 2-3 minutes rest; 5-minute break between the different Achilles tendon exercises.
The number of repetitions per set should be performed with additional weight such that the specified number of repetitions is the maximum, i.e., you should not be able to do more repetitions, otherwise, the additional weight would have been too low.
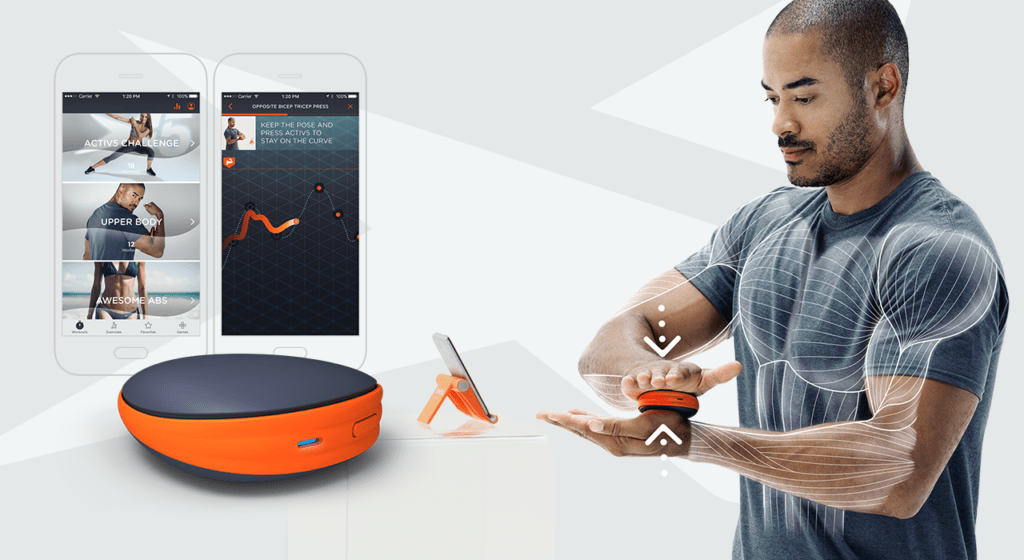
5. Achilles sensorimotor exercise – Coordination
This exercise would be best performed at first under the guidance and explanation of your physiotherapist and/or coach.
At home, the following exercises for the Achilles tendon can be performed:
- One-legged stand in different variations: with arm exercises, with eyes closed.
- Two- or one-legged stand, with various arm exercises on a soft surface, e.g., a Balance Board, Skimmy, or therapeutic floor, with eyes closed.
- Exercise motor skills for sport, these are coordination exercises that have something to do with your sport and are intended to introduce you back to your sport after a break:
– perform ABCs for joggers (i.e. skip running, kicking, side running, changes of direction, etc.).
– exercises with the ball with foot and head for footballers.